Integration of Oral Health and Primary Care: Communication, Coordination and Referral


Since the beginning of the coronavirus pandemic, older adults have been at greater risk of serious illness, hospitalization, and death due to COVID-19. In December 2020, the FDA issued Emergency Use Authorizations for two COVID-19 vaccines. At the time, the CDC Advisory Committee on Immunization Practices (ACIP) issued recommendations to give the highest priority to health care workers, and residents and staff in long-term care facilities. In mid-January 2021, the Trump Administration advised states to expand vaccine eligibility to people ages 65 and older – a population totaling more than 54 million, in addition to residents of long-term care facilities – in order to reach a broader population of high-risk individuals. This recommendation was reinforced by the Biden Administration. In response, many states changed their vaccination plans and started vaccinating adults 75 and older (consistent with ACIP recommendations), before expanding to include adults 65 and older. As of February 22, 2021, most states (41) and the District of Columbia have expanded eligibility for COVID-19 vaccines to include people 65 and older (Appendix Table 1).
Although demand for COVID-19 vaccines continues to outstrip supply, the pace of COVID-19 vaccinations nationwide is increasing, with average daily vaccinations rising from 1.1 million per day in mid-January to 1.7 million per day as of February 17, 2021. According to the CDC, more than 45 million people, or about 14% of the US population, have received at least one dose of a COVID-19 vaccine. Among adults 65 and older, the vaccination rate is considerably higher at about 41%, according to the CDC and our estimates based on 2019 Census data and long-term care facility data. In fact, people 65 and older, including residents of long-term care facilities who are primarily in this age group, account for more than half (54%) of all people who have received at least one COVID-19 vaccine dose to date.
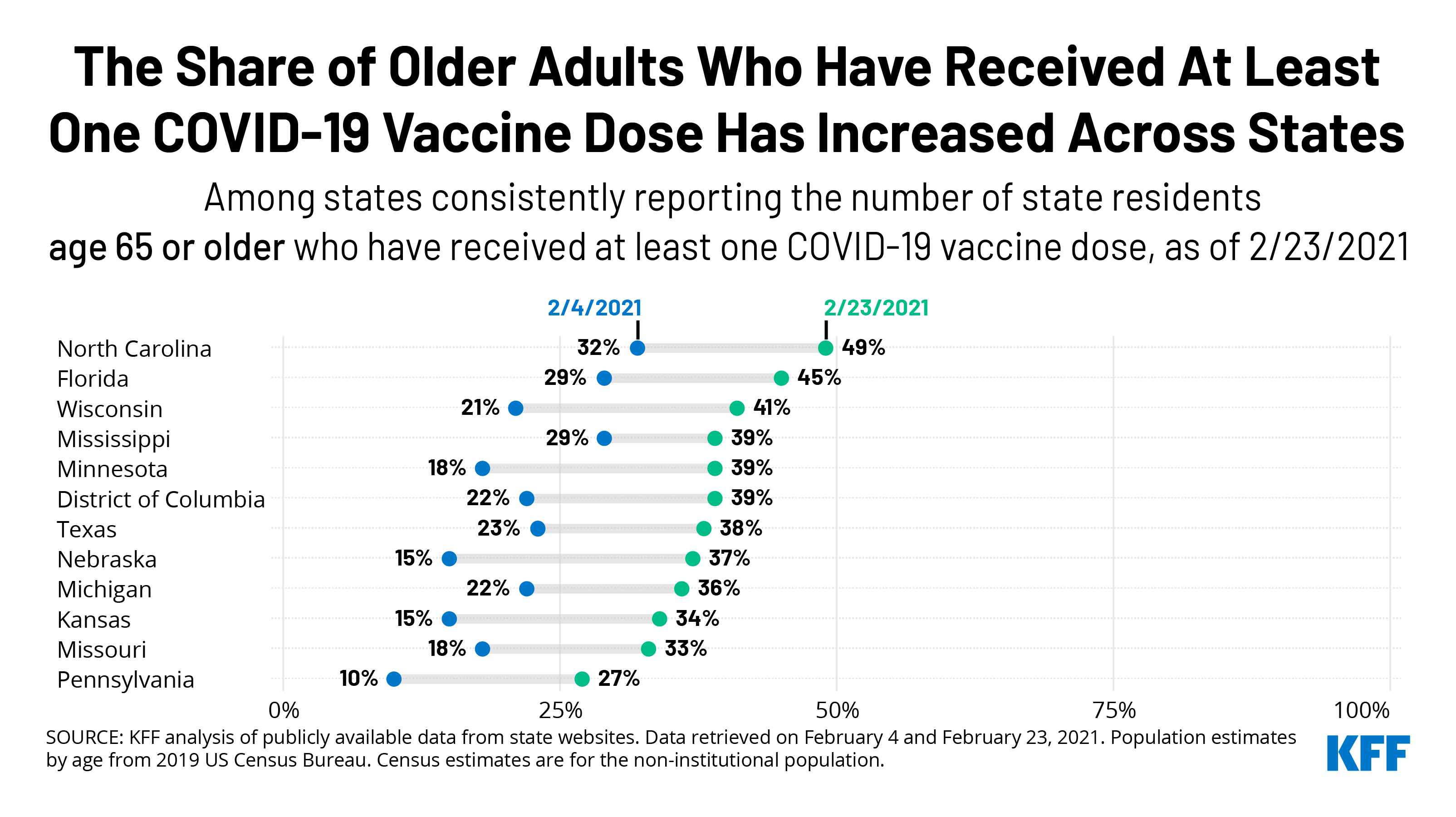
This analysis examines COVID-19 vaccination rates among older adults in the 33 states and DC that reported these data at the person-level as of February 23, 2021 (Figure 1). It also looks at the change in vaccination rates between February 4 and February 23 among a subset of these states (18 and DC) that reported consistently at both points in time. The analysis includes states reporting vaccination data by age where the data reflect the number or share of people who have received at least one dose of the vaccine; we exclude states that report the number or share of doses administered (California, Delaware, Illinois, Iowa, Nevada, New Jersey, and Virginia; see methods). Of the 33 states and DC in our analysis, 28 states plus DC have expanded vaccinations to adults 65 and older; five states have not expanded eligibility to people ages 65 and older (Kentucky, Maine, New Mexico, Oregon, and Vermont). Most of these states (21 and DC) report vaccinations among adults 65 and older, while 12 report for adults 60 and older. We report results separately for these two groups.
Of the 33 states and DC in our analysis, 22 states and the District of Columbia have vaccinated at least one-third of older adults, but no state has reported crossing the 50% threshold (Figure 2). Among the 21 states and DC reporting data for people 65 and older, 4 states report vaccinating a larger share of their 65 and older population than the national average, which is 41% (North Carolina, Florida, Arizona, South Carolina). The share of adults 65 and older who have received at least one dose of the vaccine ranges from 49% in North Carolina to 27% in Pennsylvania. The relatively low rate in Pennsylvania may be partly explained by data not included from Philadelphia county.
Two states – Florida and Texas – included people ages 65 and older in the initial prioritization group (that is, before the federal government advised including them) and report vaccination rates by age. (A third state, Georgia, also vaccinated older adults from the outset but does not report vaccination rates among older adults.) As of February 23, Florida has a higher vaccination rate among older adults than Texas (45% vs. 38%). The lower rate in Texas may be due in part to delays resulting from the recent winter storm that wreaked havoc on the state.
Among the 12 states that report COVID-19 vaccinations for people ages 60 and older, two states (Alaska and Indiana) report vaccinating more than 41% of people 60 and older. The share of adults 60 and older who have received at least one dose ranges from 49% in Alaska to 21% in Oregon.
Between February 4 and February 23, vaccination rates among older adults have increased across states that reported consistently at both points in time, with increases ranging from 10 to 22 percentage points (Figure 3). The share of adults ages 65 and older who have received at least one dose of the vaccine has increased by 20 percentage points or more in Nebraska (15% to 37%), Minnesota (18% to 39%), and Wisconsin (21% to 41%). Over this time period, Mississippi had the smallest increase among states reporting vaccinations for people 65 and older, at 10 percentage points (29% to 39%). We were able to track trends for 18 states and DC but were unable to track trends for all states that report vaccination rates (for additional information, see methods).
Among the states reporting vaccination rates among people 60 and older, South Dakota had the largest increase in the share of older adults vaccinated (16% to 36%), while Oregon had the smallest increase (11% to 21%).
Older adults account for a majority of people who have received vaccines in more than half of the states in our analysis, based on the total number of people in the state who have received at least one dose (Figure 4). Among the 21 states and DC reporting vaccinations among people 65 and older, this population accounts for half or more of all people receiving at least one dose in DC and 11 states (Florida, North Carolina, South Carolina, Alabama, Mississippi, West Virginia, Connecticut, Arizona, Ohio, Michigan, Washington). The share of all people who have received a first dose who are 65 and older ranges from 76% in Florida – which likely reflects Florida's decision to prioritize the 65 and older population before the revised federal guidance was announced – to 33% in Pennsylvania. The relatively low rate in Pennsylvania may be partly explained by data not included from Philadelphia county.
In the 12 states reporting vaccinations by age for adults 60 and older, this age cohort accounts for half or more of all people who have received one or more doses in 8 states (Indiana, Louisiana, Maine, Tennessee, South Dakota, Colorado, Maryland, Utah) ranging from 72% in Indiana to 40% in Oregon.
Very few states report vaccination rates among older adults by race/ethnicity or gender. Among the 33 states and DC that report vaccinations by age at the person level, just two (South Carolina and Washington) report both age and race/ethnicity. Based on data from South Carolina and Washington State, older White adults have been vaccinated at higher rates than older Black adults. In South Carolina, 37% of White adults ages 65 and older have received at least one dose of a COVID-19 vaccine, as compared to 28% of Black adults ages 65 and older. In Washington State, 23% of all White adults 65 and older have received at least one dose of the vaccine, but only 16% of Black older adults and 19% of Hispanic older adults have been vaccinated.
The dearth of vaccination data for older adults by race/ethnicity in most states makes it more difficult to determine how best to direct resources to people who are disproportionately affected by the pandemic or are currently experiencing vaccine access issues. Only three states (Arizona, South Carolina, and Texas) report vaccination rates among the 65 and older population by gender.
As of February 23, 2021, the majority of states have expanded eligibility for COVID-19 vaccines to include people ages 65 and older, and according to CDC and our estimates, about 41% of older adults have had at least one dose. Our analysis of state-level data shows a fair amount of variation across states that are reporting vaccination data by age. At the high end, 4 states report that more than four in 10 adults ages 65 and older have received a COVID vaccine dose, above the national average. Among states that have reported vaccination rates among older adults consistently over the past few weeks, it is clear that progress is being made in vaccinating older adults, with some states making more headway than others, as supply remains a concern.
The variation in vaccination rates among older adults across states may be due to a number of factors, including timing (when they first expanded eligibility to people 65 and older), the supply of vaccines received relative to their older population, the ability of states to increase the number of vaccinations per day, and sign-up procedures that vary across states, and within states across counties. These variations contribute to a host of problems older adults have encountered getting vaccinated, including not knowing how to schedule appointments or where to get vaccinated, waiting in long lines, or arriving for an appointment to find vaccines no longer available. Underlying inequities in resources, such as access to technology and transportation, may further increase barriers to vaccination for seniors of color.
In general, our analysis shows that states have made progress in vaccinating older adults in recent weeks amidst ongoing concerns about an insufficient supply of vaccine, but there is still a way to go before a large majority of this population has been vaccinated.
| This analysis uses publicly available data from state websites pertaining to vaccine administration retrieved on February 23, 2021. Population estimates by age for each state come from the 2019 US Census Bureau. There are some data limitations. States report vaccinations differently. States vary in whether they report the number of people who have received at least one vaccine dose, people who have received one dose and people who have received two doses, or total vaccinations administered. Where possible, we report data for the total number of people who have received at least one vaccine dose. However, some states only report total doses administered for age data, meaning people who have received two doses may be included in the data twice, and therefore are excluded from this analysis. It is not possible to calculate the overall share of older adults in the US who have received at least one dose of the COVID-19 vaccine based on state-level data in California, Delaware, Illinois, Iowa, Nevada, New Jersey, and Virginia. Further, North Dakota only reports percentages and not data on underlying counts of people vaccinated, and are also excluded from this analysis. As of 2/23/21, Pennsylvania's vaccine dashboard data does not include data from Philadelphia county due to differences in reporting criteria. States also vary in the age increments they report, with some reporting data for those 65 and older with others reporting 60 and older. Tennessee reports data for adults 61 and older. Hawaii reports age data for adults 75 and older and are not included in this analysis. We were not able to track the share of older adults who have received at least one dose of the vaccine from February 4 to February 23 in all states, either because the methodology used to report vaccination rates changed over time (Colorado, Indiana, West Virginia), the age cohort reported changed over time (Massachusetts, Ohio, Rhode Island, Vermont) or because they did not report vaccination rates among older adults as of February 4 (Alabama, Arizona, Connecticut, Kentucky, New Mexico, South Carolina, Utah, Washington). State-level data may or may not include doses delivered and administered from the Retail Pharmacy Program, the Federally Qualified Health Centers Program, and Federal Emergency Management Agency (FEMA) community vaccination sites. States also vary in whether their age data include long-term care facility residents. Currently, only six states (Alabama, Kentucky, Massachusetts, Maine, Mississippi, Nebraska) explicitly state that their age data include data from the Pharmacy Partnership for Long-Term Care and other long-term care facilities. Michigan specifies that data on long-term care vaccinations are not fully captured in their age data. North Carolina also specifies that data on doses administered as part of the Partnership are not reflected in their age data. The remainder of the states either do not specify whether their age data include data from long-term care facilities, or in others, it was unclear based on the description. According to CDC data, nearly 2 million residents of long-term care facilities received at least one dose of the vaccine nationwide, most of whom are presumably older than age 65. If states do not take into account long-term care residents who have been vaccinated, the shares reported here may somewhat understate the total share of older adults that have received at least one dose in those states. Finally, it is possible that the estimates of vaccination rates based on state websites may be low if there is a lag in reporting by states. |
Comments
Post a Comment